Cervical cancer is a silent killer targeting women in India. Even though most commonly diagnosed in women between the ages of 35 and 44, it can affect women of all age groups. At least 75,000 Indian women die of cervical cancer annually with the disease contributing to approximately 6–29% of all cancers in women.
India accounts for nearly one-third of the world’s cervical cancer deaths due to a lack of awareness and inadequate screening practices. According to data from The Indian Express, between 2017 and 2022, a total of 3,941 women in Maharashtra died from cervical cancer, with over 657 deaths per year on average.
What is Cervical Cancer?
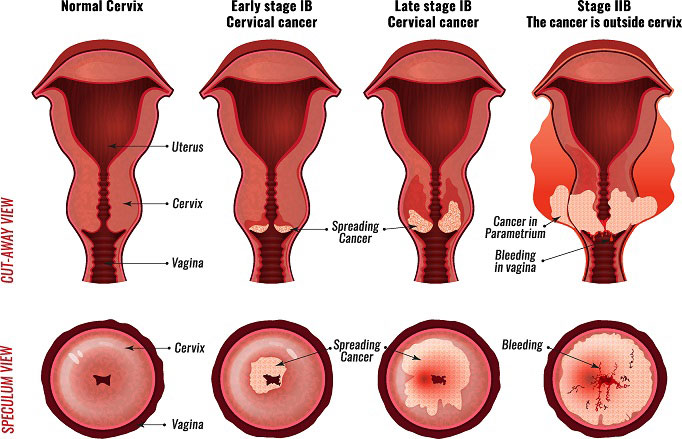
The World Health Organization (WHO) defines cervical cancer as a disease caused by abnormal cells growing in the lining of the cervix. Cervical cancer develops in a woman’s cervix, the lower part of the uterus that connects to the vagina.
Almost all cervical cancer cases (99%) are linked to infection with high-risk Human Papillomaviruses (HPV), an extremely common virus transmitted through sexual contact. Although most infections with Human Papillomavirus or HPV resolve spontaneously and cause no symptoms, persistent infection can cause cervical cancer in women.
The WHO says, “With a comprehensive approach to prevent, screen and treat, cervical cancer can be eliminated as a public health problem within a generation.”
India accounts for 27 percent of the global deaths due to cervical cancer
Cervical cancer is the fourth most common cancer in women across the world according to the WHO. In 2022, an estimated 660,000 women were diagnosed with cervical cancer worldwide and about 350,000 women died from the disease.
“Cervical cancer, which is caused by HPV or Human Papillomavirus, is a serious health concern in India in the present day. One woman succumbs to this cancer every 8 minutes. What is surprising is that more than 1 lakh 23,000 cases are detected every year. Talking about global deaths, India accounts for 27 percent of the global deaths,” Dr. Deepika Chandhok, Founder President Swasthya Vriksha Foundation told The CSR Journal.
“Awareness about cervical cancer is an absolute need of the hour today. There are a lot of questions in people’s minds such as what cervical cancer is, how it happens, how it can be prevented, how it can be cured and what role a vaccine plays in its prevention. It is necessary to address these questions and to bust the myths related to cervical cancer. The HPV vaccine is like a sanjeevani booti for cervical cancer prevention which has been approved by the World Health Organization. Crores of women aged 20 or above are being safely administered this vaccine across the world,” she informed.
Cervical cancer is curable
Cervical cancer is one of the most successfully treatable forms of cancer, as long as it is detected early and managed effectively. Cancers diagnosed in late stages can also be controlled with appropriate treatment and palliative care.
This form of cancer is preventable through routine screenings and the HPV vaccine. Effective primary (HPV vaccination) and secondary prevention approaches (screening for, and treating precancerous lesions) can prevent most cervical cancer cases.
Government of India’s initiative to prevent cervical cancer
The World Health Organization (WHO) has approved the HPV vaccine and recommends it as part of routine vaccinations in all countries. The WHO’s primary target population is girls aged 9–14 years. Despite being preventable, this form of cancer unfortunately has a high mortality rate in our country.
 Finance Minister Nirmala Sitharaman, during the interim budget presentation in February 2024, announced the Centre’s plan to include the HPV vaccine to prevent cervical cancer in the national immunization programme.
Finance Minister Nirmala Sitharaman, during the interim budget presentation in February 2024, announced the Centre’s plan to include the HPV vaccine to prevent cervical cancer in the national immunization programme.
The vaccination programme will be for girls in the age group of 9 to 14 years for the prevention of cervical cancer. However, almost a year later this is yet to be implemented.
Currently, HPV vaccines that are available in India include Gardasil (quadrivalent) and Cervarix (bivalent), which cost Rs 2,800 and Rs 3,299 per dose, respectively. Cervavac is India’s first locally produced vaccine, created by the Serum Institute of India.
Risk factors for cervical cancer
There are certain risk factors that make a person who has a high-risk HPV infection of the cervix to develop cervical cancer. These include:
Family history
This makes a person more vulnerable to cervical cancer.
Weakened immune system
This can lower the body’s ability to fight an HPV infection. HPV infections are more likely to be persistent and progress to cancer in people who have a weakened immune system. Normally, HIV infection and certain diseases weaken our immune system. Certain medicines also suppress our immune response.

Smoking
Both active and passive smoking increases cervical cancer risk.
Reproductive factors
The use of oral contraceptives (birth control pills) and giving birth to many children can increase the risk of cervical cancer.
Obesity
Cervical cancer screening may be more difficult in those with obesity, leading to lower detection of precancers and a higher risk of cancer.
DES
Diethylstilbestrol (DES) is a synthetic form of estrogen, a female hormone that was prescribed to pregnant women in the United States between 1940 and 1971. DES was used to prevent miscarriage and premature labor but was later found to be ineffective. DES exposure increases the risk of developing a rare form of cervical cancer called clear cell adenocarcinoma by 40 times.
Being exposed to DES in the womb is an independent risk factor for a type of cervical cancer called clear cell adenocarcinoma. Women whose mothers took DES while pregnant have an increased risk of cervical cell abnormalities and clear cell adenocarcinoma of the vagina and cervix.
How to prevent cervical cancer?
As discussed above, cervical cancer is preventable and curable if diagnosed early. Following are some ways in which cervical cancer can be prevented:
HPV vaccine
The HPV vaccine is highly effective at preventing HPV infection, cervical cancer, and other HPV-related cancers. The American Cancer Society recommends that children start receiving the HPV vaccine as early as 9 years. The vaccine is given in three doses over about nine months, but children under 15 only need two doses.
Regular screenings
Screening tests from time to time can help detect changes that could become precancer or cervical cancer. It is recommended that people aged 25–65 who have a cervix and are at average risk get a primary HPV should get screened every five years. If a primary HPV test isn’t available, co-testing (HPV testing plus a Pap test) every five years, or a Pap test alone can be done every three years. Irregular screening, often due to limited access in rural areas, is a problem in India.
Quitting smoking
Smoking increases the risk of precancerous conditions and cervical cancer. So, if you are a smoker, it is time to call it quits!

Safe sex and pregnancy
Using condoms during sex can help prevent cervical cancer. Condoms, which prevent some sexually transmitted diseases, can decrease the risk of HPV transmission. However, they do not completely prevent it. Therefore, exposure to HPV is still possible in areas that are not covered by the condom. Also, not having more than one sexual partner can reduce one’s risk of contracting the HPV virus. Multiple pregnancies may also increase the risk of cervical cancer.
Proper diet and workout
It is recommended that foods high in antioxidants and other cancer-fighting nutrients should be made a part of day-to-day diet. Diets high in saturated and trans fats, sugar, and sodium should be avoided. Studies show that working out for at least 30 minutes a week can help prevent cervical cancer.
Cervical Cancer Treatment
Cervical cancer treatment depends upon the stage of cancer and the patient’s health condition. In the early stage, cancerous tissues can be removed through surgery. Hysterectomy is used for more advanced cases, involving the removal of the uterus and cervix, while Radical hysterectomy may be required depending on the spread of the cancer. Other types of treatment include Radiation Therapy, Chemotherapy, Targeted Therapy and Immunotherapy.
Ahana Bhattacharya can be reached at ahana@thecsrjournal.in


